Anywhere from 1.6 to 2.8 million concussions may occur each year across the U.S.1 Trauma facilities across the nation see such injuries all too often, as traumatic brain injury (TBI) occurs at a high frequency. Often a consequence of a concussion, which is itself a brain injury, TBI accounts for 30% of all injury deaths in the U.S. There were about 2.8 million visits to the ER, hospitalizations, and deaths in 2013 due to TBI.2
The Latin root of the word concussion is concutere, meaning “to shake violently.” That is exactly what happens to the brain with a blow to the head (or body), which may occur because of a fall, athletic injury, or car crash. A fight or a work-related injury can cause a concussion as well.
How Hard Do You Have to Hit Your Head to Get a Concussion?
The truth is you don’t have to hit your head at all. Sudden and violent motion can cause the brain to shake rapidly. Made of soft tissue (with the consistency of gelatin), the brain is cushioned inside the hard skull by cerebrospinal fluid. A jolt to the brain can cause it to shift, causing bruises and nerve and blood vessel damage.
Anyone can get a concussion, but young children are more susceptible because their heads are disproportionately large. They may not be able to verbalize how they feel, so it’s important to watch them for behavioral changes that might indicate a brain injury.
According to the Centers for Disease Control and Prevention, most TBIs and concussions are caused by falls. Data from 2013 show over half of hospital visits and deaths in children related to TBI were due to a fall, as were 79% of TBI-related visits and deaths in adults over 65. The second leading cause was being hit by an object, with motor vehicle crashes the third most common cause of brain injuries. Falls and intentional self-harm were also factors.3
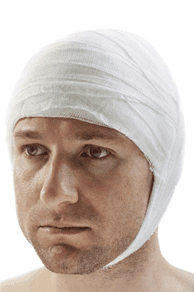
Signs of a Concussion
A direct blow to the head or violent shaking of the upper body can disrupt the function of the brain. As a result, a person can black out or fall unconscious, but this is not as common as one might think. The most common symptoms to look for are the following:
- Dizziness and loss of balance
- A dazed or confused feeling
- Memory loss following the event (amnesia)
- Difficulty concentrating
- Personality/behavioral changes
- Light and sound sensitivity
- Blurry vision
- Ringing in the ears
- Headache
- Seizure
- Sluggishness
- Insomnia or other sleep disturbances
A concussion victim may have trouble sleeping or even difficulty awakening from sleep. More serious signs also include enlarged pupils or pupils that are unequal in size. If a progressively worsening headache, nausea/vomiting, bizarre behavior, slurred speech, numbness or weakness in the extremities, or fainting occur, seek medical help or immediately call emergency services (such as those provided by our Texas injury center).
Children should be closely monitored if a concussion is suspected. For those under two who experience a fall or other trauma, look for swelling and abnormalities on the scalp. Changes in behavior can indicate a problem as well. Medications should not be given to them unless a doctor advises it; for example, aspirin can trigger bleeding.
The symptoms vary with the person and the injury, but a young child may not be able to accurately explain how they feel. Although symptoms last three to ten days, they may last longer in children and teenagers, as well as people who have had multiple concussions. The following signs may indicate head trauma in a young child, infant, or toddler:
- Irritability
- Easily tiring
- Listlessness
- A dazed look
- Loss of balance
- Trouble walking
- Changes in habits (i.e., eating, sleeping)
- Excessive crying
- Disinterest in play or toys
If your child experiences a head injury, he or she should visit the doctor in a day or two, even if a trip to the ER isn’t required, the Mayo Clinic advises. A nap is okay if there are no signs of a head injury and the child is responsive and alert. At any age, a concussion can be caused by:
- A blow to the head, neck, or upper body, causing the brain to slide back and forth.
- Sudden acceleration and deceleration, which can easily injure the brain.
- A fall, motor vehicle accident, or any athletic or recreational activity.
In many cases, brain function is disrupted only briefly. A TBI can also trigger bleeding near or within the brain, leading to more severe, prolonged symptoms. Sometimes the symptoms do not occur right away. If symptoms worsen, it should be considered an emergency, and treatment at one of our trauma facilities is critical. Any amount of brain bleeding can be fatal.
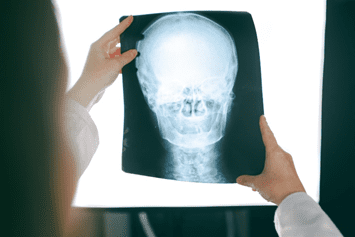
How a Concussion Is Diagnosed
To diagnose a concussion, a doctor will assess the individual’s symptoms and conduct neurological tests. The patient’s motor and sensory skills, cranial nerve function, speech, vision, hearing, coordination/balance, and mental state will be examined.
A physician may also ask about any changes in mood or behavior or start with very simple questions such as the person’s name and where they live. If a neurological exam reveals any symptoms, the next step is typically a medical scan at our Texas injury center.
A computerized tomography (CT) scan provides a detailed look at the brain and can identify areas of swelling or bleeding. Alternatively, a magnetic resonance imaging (MRI) test, using magnetic energy, yields detailed pictures that can determine whether a TBI has occurred or not. Even if a scan is negative, the damage may not be visible. Precautions should, therefore, be taken as recommended by a doctor as one recovers.
Concussions are categorized as different types, such as:
- Grade 1: Mild concussion, with symptoms lasting less than 15 minutes.
- Grade 2: Moderate concussion; symptoms last more than 15 minutes, with no loss of consciousness.
- Grade 3: The victim experiences a loss of consciousness, which can last just seconds or longer.
An individual with a grade 1 or 2 concussion may have symptoms for minutes to hours or days; sometimes they last for up to a week. See a doctor immediately for a grade 3 concussion.
What to Do After a Concussion
It is important to follow a doctor’s advice for recovery; sometimes, overnight hospitalization is necessary to observe whether symptoms persist or worsen. Treatment for a concussion often includes aspirin-free medication and rest. An athlete is strongly advised to take a break from sporting activities, while a thorough evaluation is performed by coaches to determine whether someone is ready to resume full activity.
For anyone with a concussion, rest from physical activity, including aerobic exercise and heavy lifting, is recommended. Mental rest is important, too. This includes avoiding television, video games, reading, and text messaging, or other activities that require a high degree of mental focus. Driving is not recommended, either, as it requires much concentration, and reaction time may be decreased.
Rest is important as the brain heals. Brain recovery occurs mostly during sleep, so get a full night’s sleep and take short naps when necessary. Short 30 to 60 minute naps are fine when tired, and these are important in helping the brain recover. Children who come home from school and finish their homework, after a concussion, will be exhausted from these activities. Students should alert their teachers of an injury and discuss modifying assignments during the recovery period.
In any case, at any age, people should not return to normal activities unless their symptoms have abated or a doctor has given the okay. Severe bleeding and swelling may require emergency surgery, although the majority of concussion cases require mainly rest and avoidance of activities that trigger symptoms. If any activity triggers symptoms, it should be stopped immediately.
Repercussions of Not Getting Prompt Care
The symptoms of a concussion, or even mild TBI, usually don’t last more than a week or two. The prognosis is usually positive. However, prompt diagnosis is essential. You might have to convince a family member or friend to seek medical attention at trauma facilities, but you may be saving their life.
Bleeding and swelling in the brain often don’t have symptoms until it’s too late. The after effects can range from physical and cognitive impairment to stroke, coma, and death, although bleeding and blood clots occur in just 5% of individuals who suffer a concussion.4
General complications of a concussion, and not getting prompt care, include:
- Post-traumatic headaches lasting from a week to a few months.
- Post-traumatic vertigo, or a feeling of dizziness or spinning.
- Post-concussion syndrome consisting of difficulties with balance, pain, and thinking.
People who have had multiple brain injuries face a higher risk of lasting impairments. The risk of progressive difficulties is higher in those who have sustained head injuries before, no matter what point in their life they occurred. A second concussion, while the brain is still healing from the first (and symptoms are still present) may cause fatal brain swelling. Remember, a concussion affects the brain physically and chemically, so you want to avoid additional injury as much as possible.
Preventing head injury, whether one has had a TBI in the past or not, is possible. It may at least minimize the risk of sustaining trauma. Preventative measures include:
- Wearing well-fitting maintained protective gear for sporting and recreational activities.
- Wearing a seat belt in a car, which minimizes the risk of head injury during an accident.
- Eliminating causes of trips and falls and having adequate lighting at home.
- Installing window guards and bunkbed rails and blocking stairways for small children.
- Getting regular exercise to improve balance and strengthen leg muscles.
- Spreading awareness of the risk and dangers of concussions.
Visit Exceptional Emergency Center
Our Texas injury center is one of the most equipped and professionally staffed trauma facilities in the region. If you, a child, friend, or loved one has sustained a head injury, visit us for emergency care; acute treatment is provided in specially equipped rooms, while advanced imaging services are available. We’re equipped with x-ray, CT scan, and ultrasound machines, and we have experience treating critical injuries. Our team is also trained and experienced in pediatric emergency care.
To reach us in an emergency, contact us 24/7 at our regional facilities:
Harlingen, TX: 956-567-0371
East Chase, TX: 817-566-0285
Dow Emergency–Livingston: 936-327-7000
Excellence ER–Sachse: 469-202-8658
Your prompt action can save a life or prevent lasting impairments, so call one of our trauma facilities ASAP.


